- Diseases of the retina and age-related degeneration can lead to impaired vision.
- Scientists working on restoring sight are developing multiple promising solutions.
- These techniques bypass damaged retinas with a variety of alternate approaches that convince the brain to see.
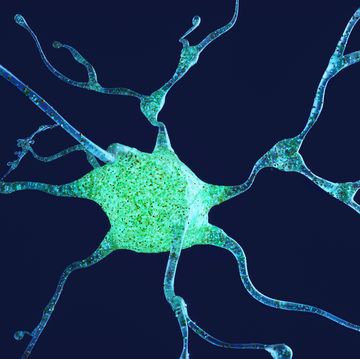
The human retina—the light-sensitive part of the brain situated in the back of the eye—is a feat of engineering at the heart of a critical sense: Sight. So diseases of the retina like retina pigmentosa or age-related macular degeneration, which lead to impaired vision and blindness, can be particularly intractable and devastating.
But scientists are zeroing in on a suite of strategies that may offer a ray of hope.
👁 New technologies are amazing. Let’s nerd out over them together.
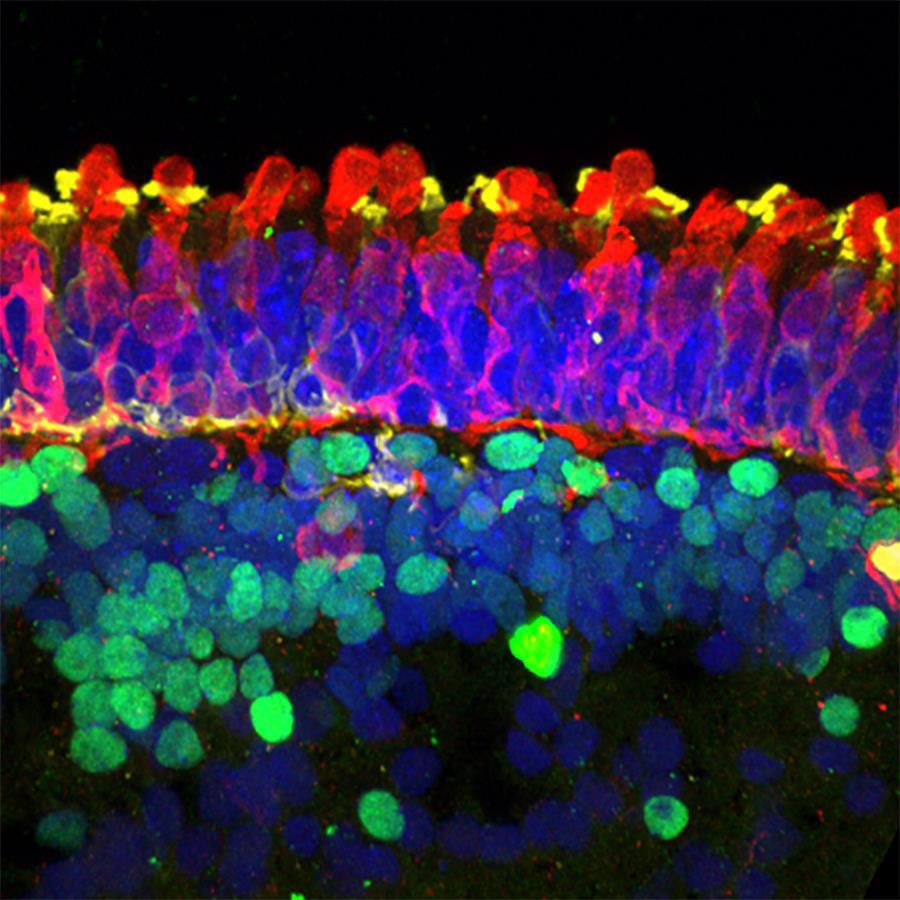
Exquisitely organized, the retina detects light from the environment around us and transforms it into electrochemical signals that ultimately reach the brain’s visual cortex, where they’re further processed and interpreted into images we can understand. But damage to any part of the system—from the light-sensitive photoreceptors to the bipolar cells they communicate with to the ganglion cells that transmit this information via the optic nerve to the brain—can eat away at our vision.
While there are myriad strategies to restore sight, retinal prosthetics, or electrode arrays implanted on or in the retina, have made the most headway. Bypassing damaged photoreceptors, the electrodes directly stimulate surviving neurons—either bipolar or ganglion cells—that feed into the brain’s visual cortex, imparting an artificial version of sight to patients. Most setups include a camera mounted on glasses that takes in images, which are translated into electrical signals by a processor. These signals are then sent to the electrode arrays.
Current technologies, however, can’t replicate the activities of the retina, which is a complex microprocessor with multiple synaptic stages, condensing information from 120 million photoreceptors to 1.2 million ganglion cells, says Diego Ghezzi, a professor of neuroengineering at the Ecole Polytechnique Fédérale de Lausanne in Switzerland. And the retina’s exact output to the brain—the spatiotemporal patterns of electrical pulses generated by the ganglion cells—is unknown. “So, since we do not have technology that can individually reproduce perfectly this code in 1.2 million retinal ganglion cells, what we do is an approximation,” Ghezzi tells Popular Mechanics.
A Prosthesis for the Eye
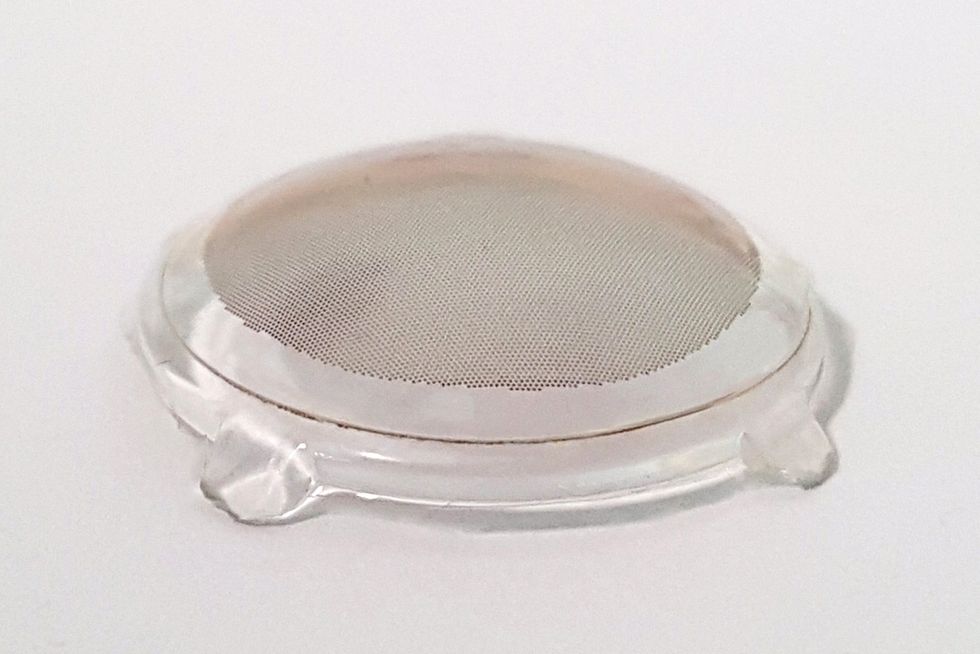
Ghezzi’s team has devised a photovoltaic retinal prosthesis, which functions similarly to the Argus II, the now discontinued prosthesis that had been in use since 2011. “The big difference is that our electrodes, like solar panels, are capable of absorbing light and converting it into electricity within the device,” Ghezzi says. And while glasses, amplifying ambient light to an intensity that the prosthesis can detect, are still necessary, Ghezzi’s system comes with several improvements over previous technologies.
“Visual acuity is limited by the distance between electrodes,” says Ghezzi. “In our device, that distance is 120 microns [compared to 575 microns in the Argus II], which corresponds to a visual acuity of 20/480.” Additional tricks, however, can boost this number. “You can zoom in with the glasses—so if you have to look at very tiny things like a textbook page, zooming can increase your resolution from 20/400 to 20/200, for example.” But this trick is performed at the cost of cutting into the visual field, or the area that’s visible when you fix your gaze.
Experiments and simulations have shown that a visual angle of at least 30 degrees is necessary for functional mobility, or the ability to safely move through an environment. Ghezzi’s aim, therefore, was to “have a good enough visual acuity paired to a very large visual angle.”
Composed of 10,498 pixels and covering a visual angle of 43 degrees, his team’s prosthetic represents a marked improvement over the 20 degrees achieved by the Argus II; and because it’s constructed with flexible organic polymers, it conforms naturally to the eye’s curved surface. The researchers recently tested the device in Göttingen minipigs, demonstrating that the implanted prostheses respond to light. The next step, Ghezzi says, is to test the implant in humans.
Sound Waves That Can Stimulate Vision
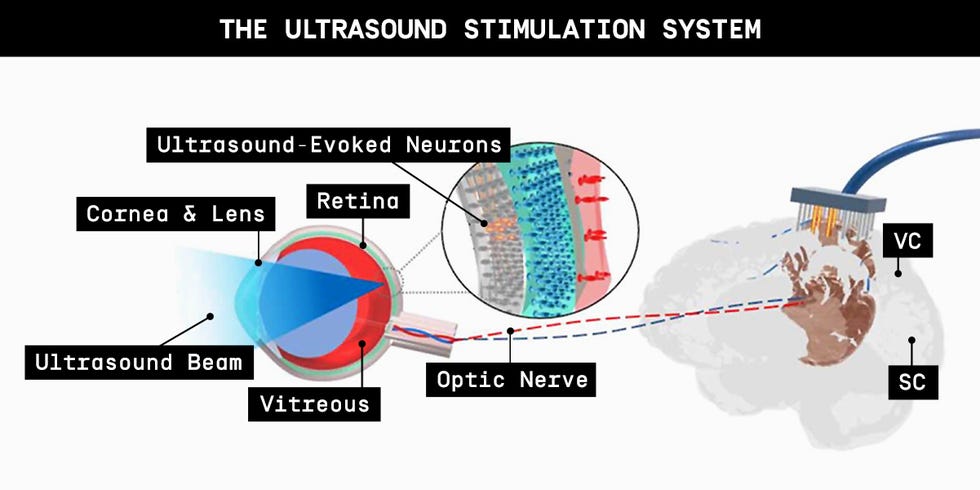
Other scientists, like Qifa Zhou at the University of Southern California, have approached the problem from a different tack. Rather than stimulating retinal neurons from within the retina, Zhou and his colleagues triggered their activity with ultrasound, or high frequency sound waves, that originate outside of the eye.
“With electric stimulation, surgeons need to put the electrodes inside the eye; it’s an invasive technology,” Zhou tells Popular Mechanics. “Our method is potentially less risky.” Like other retinal prosthetics, Zhou’s set-up would incorporate a camera that receives images and processes them into a pattern—in this case, ultrasound waves—that’s beamed into the eye. Proof of concept studies with rats linked ultrasound stimulation of the retina with electrical responses in the visual centers of the brain.
A Viral Solution
Several groups are pursuing vision restoration through optogenetics, in which retinal neurons are induced—via a virus that targets specific cells—to express light-sensitive proteins in their cell membranes. José-Alain Sahel and colleagues were the first to successfully implement this technique in patients, as reported in a paper published last year.
Although their method also requires a camera and processor to translate images from the environment into pulses of light that can excite the transformed neurons, it’s likely more reliable and versatile than traditional prostheses. Cells in the retina continue to express the photosensitive protein after a one-time injection of the virus, while physical implants could degrade and stop working, accompanied by risks of infection. “And the goggles, since they’re outside the eyes, can evolve over time,” Sahel, the Chair of Ophthalmology at the University of Pittsburgh School of Medicine and Director of the UPMC Eye Center, tells Popular Mechanics. “They’re already different from the first goggles we developed, with more to come.”
But what, in fact, do patients see?
“The type of signal that’s produced with this [light-sensitive] protein is a new type of signal and the patient has to learn how to make sense out of it,” Sahel says, comparing the process to learning a foreign language. Each pixel in the camera reacts to a change in light, so it’s like looking at a scintillating screen, where pixels flash as the light changes at that position. This neuromorphic camera, notes Sahel, is designed to partially mimic how the retina responds to light.
Signals arise, therefore, when the object moves or the patient shifts their head or their eyes in a type of edge detection, explains Sahel. Gradually, patients are able to discern shapes, light sources, edges, and objects in motion. Dan Dunfee, a patient participating in the clinical trial in Pittsburgh, says it’s like looking out of glasses smeared with Vaseline at a world bathed in different intensities of blue.
“I see contrast and light and the edges where the contrast and light change,” Dunfee tells Popular Mechanics. “And when I find what I think is an edge of something, I’ll scan around to find the other edges of it—and from that, I get a sense of size, shape, and how reflective an object is.”
The vision that results from these therapies deviate so much from natural vision because the retina responds to light in a different way than it normally does, says Stuart Trenholm, an assistant professor of neuroscience at the Montreal Neurological Institute.
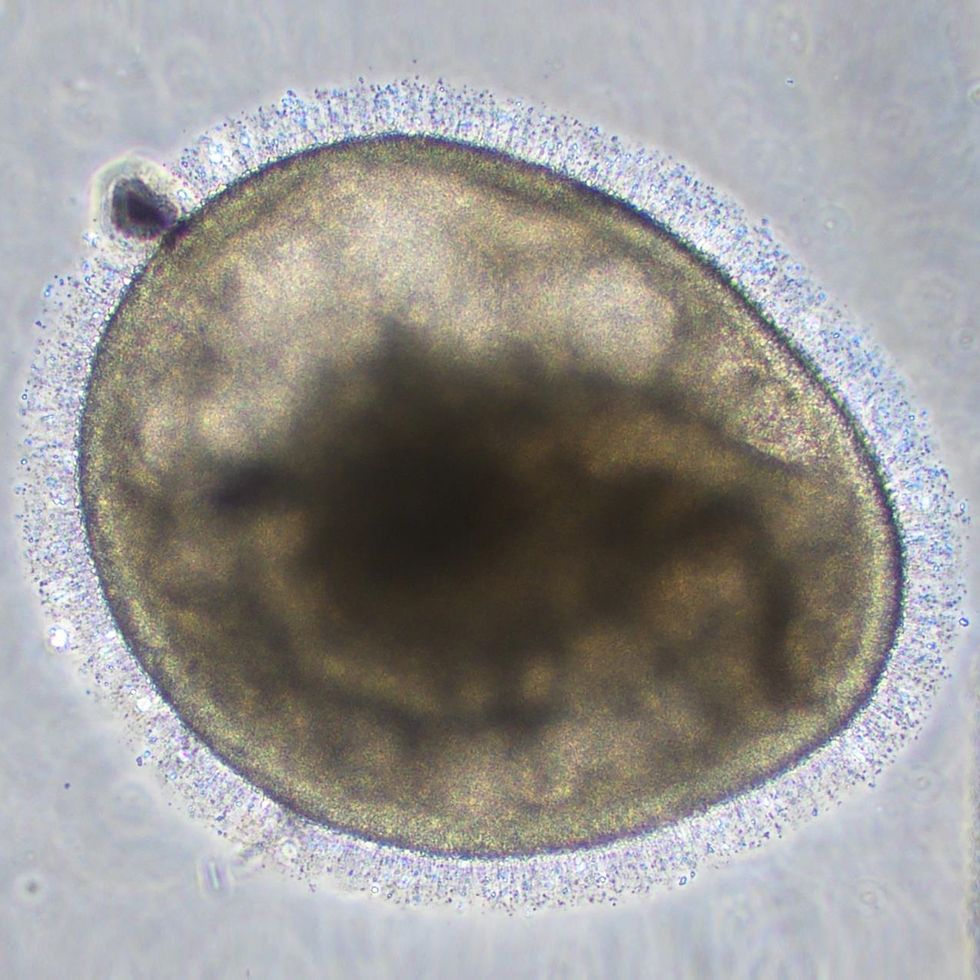
Stem Cells Have the Potential to Restore Vision
That’s where stem cell therapies, in which the body’s own cells can be coaxed to differentiate into retinal cells or even an entire retina, hold a lot of promise. “Almost like magic, the retina in a dish, or a retinal organoid, seems to grow all the different parts of the retina,” Trenholm tells Popular Mechanics. “And since so much of brain development is dependent on the surrounding environment, growing replacement parts in a whole tissue may get you more naturalistic cells,” which can then replace damaged and dead tissue.
David Gamm, a professor and pediatric ophthalmologist at the University of Wisconsin, likens the process to manufacturing spare parts for a car. “We can make spark plugs for your car, but if the engine is totally melted and rusted, new spark plugs aren’t going to do it,” he tells Popular Mechanics. Similarly, patients who have lost their cones or rods but retained the rest of the underlying neural architecture, could benefit from transplanted photoreceptors, while those further along in their diseases would need greater reconstruction.
His team recently co-published research with Raunak Sinha’s lab at the University of Wisconsin-Madison, proving that cone photoreceptors in retinal organoids grown from human stem cells respond to light like macaque retinas do. Now Gamm’s on the precipice of attempting this spark plug replacement in upcoming clinical trials. “We’ve shown that the cell has that capacity to detect light and that it’s an actual, authentic cell. But can it install [itself in the right place] and pass that signal on to a native cell in that patient?”
But Gamm cautions that progress will be incremental. “If you’ve been a quadriplegic for 30 years, the idea that you’ll run a marathon after getting stem cell therapy isn’t realistic.” Similarly, Gamm believes the technology will offer small, meaningful improvements at first, such as someone who can only detect light becoming capable of sensing motion as well. “And then we’ll innovate on that.”

Connie Chang is a freelance writer in the Bay Area -- covering science, parenting and health. She's a recovering scientist, inveterate knitter and fan fiction enthusiast.